Is A Tongue Tie Ruining Your Feedings? Silent Signs You Shouldn’t Ignore
You’ve read all the books, you’ve set up your nursing station, and you were ready for this beautiful bonding experience. But now that your little one is here, feeding feels less like bonding and more like a battle. Your baby is fussy, you’re in pain, and you’re starting to wonder, ‘What am I doing wrong?’
Friend, I want you to take a deep breath and hear me: You are not doing anything wrong. As a pediatric nurse and lactation consultant, I’ve sat with countless parents who feel this exact same way. Often, the root of the problem isn’t your technique or your baby’s temperament, but a small, hidden physical issue: a tongue tie.
A tongue tie, or ankyloglossia, is a condition where the thin strip of tissue under the baby’s tongue (the lingual frenulum) is too short or tight, restricting the tongue’s movement. While some are obvious, many are ‘posterior’ or ‘hidden,’ causing a host of confusing symptoms that are easy to mistake for colic, reflux, or just a ‘fussy baby.’ This guide is here to turn down the noise and help you listen for the silent signs, empowering you with the knowledge to advocate for your baby and reclaim your feeding journey.
Decoding the Lingo: What Exactly Is a Tongue Tie?
Before we dive into the signs, let’s get clear on what we’re actually talking about. It sounds a little scary, but a tongue tie is simply a matter of anatomy. Everyone has a lingual frenulum, but for some babies, it’s overly restrictive. Think of it like a shirt that’s buttoned up too tightly at the neck—it limits movement and makes things uncomfortable.
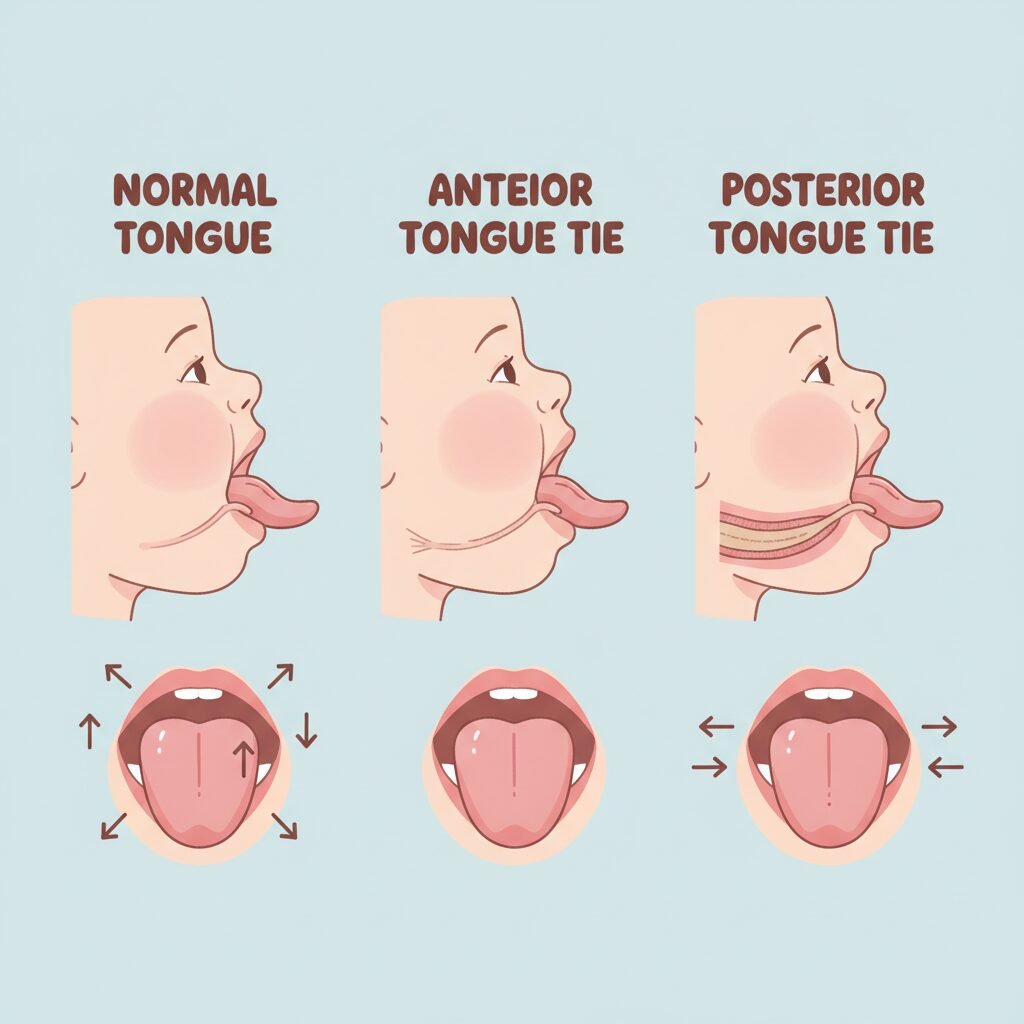
Anterior vs. Posterior: Not All Ties Are Obvious
You might have heard about different ‘types’ of tongue ties, and it’s a key reason why they’re so often missed:
- Anterior Tongue Tie: This is the ‘classic’ tie most people think of. The frenulum is attached close to the tip of the tongue, often making the tongue look heart-shaped when the baby tries to lift it or cry. It’s usually easier to see and diagnose.
- Posterior Tongue Tie (Submucosal): This is the sneaky one. The restriction is further back, hidden under the mucous membrane (the thin layer of tissue lining the mouth). The tongue might look completely normal at a glance, but its upward mobility is limited. This is often the culprit behind those ‘silent’ feeding issues because the problem isn’t how the tongue looks, but how it functions.
A Gentle Reminder: A tongue tie is a congenital condition, meaning your baby was born with it. It has absolutely nothing to do with anything you did or didn’t do during pregnancy. It’s just one of those things, and the most important step is identifying it.
Listening to Your Baby: The Silent Signs of a Tongue Tie

Your baby can’t tell you what’s wrong, but they are giving you clues all the time. A tongue tie forces a baby to work much harder to eat and to use incorrect muscles to compensate, leading to a cascade of subtle issues. See if any of these sound familiar.
Clues During Feedings:
- Shallow Latch: Does it feel like your baby is just chomping on the nipple instead of taking a deep mouthful of breast tissue? A tied tongue can’t extend and cup the breast properly.
- Clicking or Smacking Sounds: This is a classic sign! The clicking noise happens when the baby loses suction on the breast or bottle because their tongue can’t maintain a good seal.
- Frequent Detaching: Your baby may pop on and off the breast repeatedly out of frustration because they can’t draw the milk out efficiently.
- Excessive Dribbling: While some dribbling is normal, a significant amount of milk leaking from the corners of their mouth can indicate a poor seal.
- marathon’ Nursing Sessions: Is your baby feeding for 45 minutes or longer, only to seem hungry again a short while later? This points to inefficient milk transfer—they’re working hard but not getting much milk.
- Biting or Gumming: To compensate for a poor latch, babies with a tongue tie often bite down with their gums to hold the breast in place, which can be incredibly painful for you.
Clues Between Feedings:
The effects of a tongue tie don’t stop when the feeding ends. The inefficient feeding pattern can lead to other issues:
| Symptom | Why It Happens with a Tongue Tie |
|---|---|
| Excessive Gassiness or Spitting Up | A poor seal causes the baby to swallow a lot of air along with milk, leading to painful gas, bloating, and reflux-like symptoms. |
| Poor Weight Gain | This is a major red flag. If the baby is working hard but not transferring milk well, they may struggle to gain weight appropriately, despite constant feeding. |
| A ‘Lip Blister’ | You might notice a blister or callus on your baby’s upper lip. This forms because they’re using their lips to hold on, rather than their tongue creating suction. |
| Difficulty with Pacifiers or Bottles | The issue isn’t just with breastfeeding. A baby with a tongue tie may struggle to hold a pacifier in their mouth or make a clicking sound when drinking from a bottle. |
Remember, your baby isn’t being ‘difficult’ on purpose. They’re doing the best they can with the anatomy they have. These signs are their way of communicating a struggle.
It’s Not Just About Baby: How a Tongue Tie Affects You

Dear parent, your experience in this feeding journey matters just as much. A tongue tie doesn’t just impact the baby; it can take a significant physical and emotional toll on the breastfeeding mother. Your pain is real, and it’s a critical diagnostic clue.
Physical Signs for Mom:
- Severe Nipple Pain: While some initial tenderness can be normal, breastfeeding should not be excruciating. A shallow, compressive latch from a tongue tie can cause toe-curling pain throughout the feed.
- Nipple Damage: Are your nipples cracked, blistered, bleeding, or scabbed? This is a sign of trauma from an incorrect latch.
- Misshapen Nipples After Feeding: Take a look at your nipple immediately after your baby unlatches. Does it look flattened, creased, or shaped like a new tube of lipstick? This ‘lipstick shape’ is a tell-tale sign of compression.
- Low Milk Supply: Your body produces milk on a supply-and-demand basis. If your baby isn’t effectively removing milk from the breast, your body gets the signal to produce less.
- Recurrent Plugged Ducts or Mastitis: Incomplete milk drainage is a primary cause of plugged ducts, which can lead to mastitis, a painful breast infection. If you’re dealing with this over and over, it’s time to look for the underlying cause.
The Emotional Toll:
Let’s be honest: this is exhausting. When you’re in constant pain and worried your baby isn’t getting enough to eat, it’s easy to feel defeated. You might feel anxious every time a feeding approaches, frustrated with your body, or even guilty, wondering if you’re failing. These feelings are valid, but they are not a reflection of you as a parent. They are a symptom of a problem that has a solution.
You Suspect a Tongue Tie… Now What? Your Action Plan

Okay, you’re nodding along and thinking this sounds exactly like your situation. So, what’s next? Taking action can feel overwhelming, but you can do it one step at a time. The goal is to get a proper evaluation from a professional who specializes in this area.
Step 1: Assemble Your Expert Team
Not all healthcare providers have extensive training in identifying functional tongue ties, especially posterior ones. You need to find the right people. Your dream team might include:
- An IBCLC (International Board Certified Lactation Consultant): This should be your first call. An experienced IBCLC can perform a full functional assessment, observe a feeding, and determine if a tie is impacting your journey. They are invaluable guides.
- A Pediatric Dentist or ENT (Ear, Nose, and Throat) Specialist: Look for a provider who is known as a ‘tie-savvy’ or ‘tie-informed’ specialist. They are the ones who can formally diagnose and perform the release procedure, often called a frenotomy. Ask local parenting groups for recommendations!
Step 2: The Evaluation
A proper assessment is more than a quick peek in the mouth. A provider should:
- Use their gloved finger to feel under the tongue and assess its mobility and structure.
- Evaluate not just the tongue, but also the lip and cheek ties, as they often occur together.
- Watch your baby feed (at the breast or on a bottle) to see the functional challenges in real-time.
Step 3: Understanding the Treatment (Frenotomy)
If a restrictive tie is diagnosed, the recommended treatment is often a simple in-office procedure called a frenotomy. Here’s what you need to know:
- What is it? It’s a procedure where the provider uses a sterile scissor or a specialized laser to quickly snip and release the tight frenulum.
- Is it painful for the baby? The frenulum has very few nerve endings. For newborns, the procedure takes seconds and is often done without anesthesia. Most babies are more upset about being held still than the procedure itself. Many parents report their baby latched and fed more comfortably just minutes later.
- What are the risks? When performed by an experienced provider, the risks are extremely low, with minor bleeding being the most common.
Important Safety Note: Please do not try to diagnose or stretch a suspected tie on your own. A comprehensive evaluation by a trained professional is essential to get the right diagnosis and treatment plan for your baby’s specific needs.
The Other Side: Healing and Thriving After a Tongue Tie Revision

A frenotomy can feel like a magic wand, but it’s important to know that it’s the first step in a rehabilitation process. Your baby has been compensating for their entire life; now, they need to learn a whole new way to use their tongue! This is where the real work—and the real magic—begins.
The Importance of Aftercare
Your provider will give you a set of simple stretches to perform in your baby’s mouth for a few weeks after the procedure. This is the most critical part of the process. The stretches are not meant to be painful but are essential to prevent the tissue from reattaching as it heals. Think of it like physical therapy for the tongue.
| Post-Procedure Phase | Key Focus | Typical Activities |
|---|---|---|
| First 24-48 Hours | Comfort and Healing | Skin-to-skin contact, frequent feeding opportunities, pain management as advised by your provider (if needed). |
| Weeks 1-3 | Active Healing & Re-Patterning | Consistently performing prescribed stretching exercises. Follow-up visit with your IBCLC to work on latch and feeding technique. |
| Weeks 1-4+ | Bodywork & Support | Consider seeing a pediatric chiropractor or craniosacral therapist to help release tension in the jaw, neck, and shoulders caused by compensating. |
What to Expect
Some parents see an immediate, dramatic improvement in feeding. For others, the progress is more gradual. Be patient with your baby and yourself. You may notice:
- A wider, deeper latch that is no longer painful for you.
- The disappearance of the ‘clicking’ sound.
- More efficient feedings—shorter in duration but more effective.
- A calmer, less gassy baby.
- A gradual increase in your milk supply as milk is removed more effectively.
Working with your IBCLC after the procedure will help you and your baby learn your new feeding dance together. It’s a process of retraining and rediscovery that can lead to the peaceful, bonding experience you’ve been hoping for.
Conclusion
Navigating the challenges of early parenthood is tough, and feeding difficulties can feel especially isolating. If this article has felt like reading your own story, please know that you are not alone, and your intuition is powerful. Those ‘silent signs’—the clicking, the pain, the endless feedings, the fussy baby—are your baby’s way of asking for help.
A tongue tie is a common but treatable condition. By recognizing the signs and seeking out the right professional support, you can find the answers you need. You are your baby’s greatest advocate. Trust your gut, ask for help, and know that you are already an amazing parent. You and your baby both deserve a feeding journey filled with comfort, connection, and joy.







