How To Dry Up Breast Milk Supply Fast Without Getting Mastitis
Deciding to wean your baby and dry up your milk supply is a significant step, and it’s one that can be filled with a whole mix of emotions—relief, sadness, freedom, and maybe a little bit of anxiety. Hey, that’s completely normal! As a pediatric nurse and lactation consultant, I’ve sat with countless new parents as they’ve navigated this exact transition. There’s no right or wrong time, only what’s right for you and your family. My goal here isn’t to tell you when to wean, but to give you a safe, gentle, and effective roadmap for how to do it.
You’ve probably heard stories about the discomfort of engorgement or the misery of mastitis, and you’re wisely looking for ways to avoid that. The good news is, you absolutely can! The key is to work with your body, not against it. This guide will walk you through the process step-by-step, focusing on how to reduce your supply comfortably and, most importantly, how to prevent painful complications. Let’s do this together, with kindness and patience for the amazing body that has nourished your little one.
Understanding the ‘Supply and Demand’ of Breast Milk
Understanding the ‘Supply and Demand’ of Breast Milk
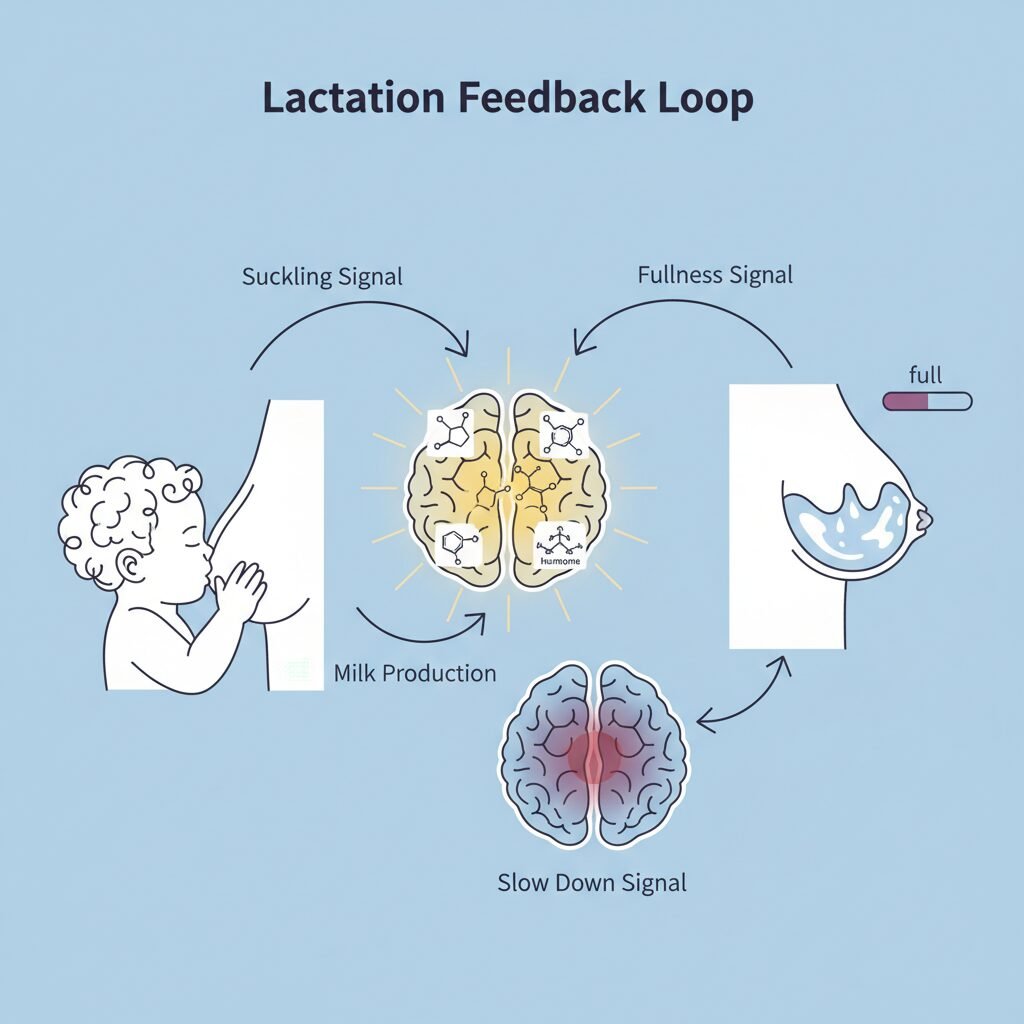
Before we dive into the ‘how-to,’ let’s have a quick chat about the biology behind it all. Think of your milk production as a beautifully simple (and incredibly smart) system of supply and demand. When your baby nurses or you pump, milk is removed. This removal sends a message to your brain: ‘Hey, the milk bar is empty! We need to make more!’ Your brain then releases hormones, like prolactin, that tell your breasts to get back to work producing more milk. The more frequently and effectively milk is removed, the louder that message is, and the more milk you make.
So, to dry up your supply, we need to reverse that process. We need to send a new message: ‘Thanks, but we’re good! You can slow down production now.’ This is done by gradually decreasing the ‘demand’—the amount of milk being removed. When milk is left in the breasts for longer periods, a protein called Feedback Inhibitor of Lactation (FIL) accumulates. FIL is like the friendly manager of the milk factory who walks around saying, ‘Alright team, we’ve got a surplus here, let’s slow things down.’ This is your body’s natural, built-in mechanism for weaning.
Why ‘Cold Turkey’ Is a Recipe for Trouble
You might be tempted to just stop breastfeeding or pumping altogether, especially if you want the process to be fast. I completely understand the impulse, but I strongly advise against it. Stopping abruptly is like slamming the brakes on that milk production factory. The ‘make more milk’ messages have already been sent, and the machinery is in full swing. If milk isn’t removed, it backs up, leading to intensely painful engorgement, where your breasts become hard, swollen, and tender. This extreme pressure can easily lead to clogged ducts and, in a worst-case scenario, mastitis—a painful breast infection that can make you feel like you have the flu. A slow and steady approach is always the safest and, honestly, the most comfortable way to go.
The Gradual Approach: Your Safest Step-by-Step Plan

The Gradual Approach: Your Safest Step-by-Step Plan
Patience is your best friend during this process. Going slowly allows your body time to adjust its production levels downward, minimizing discomfort and risk. The overall goal is to gradually reduce demand over several days or even a few weeks. Here’s how you can do it.
Step 1: Drop One Feeding or Pumping Session at a Time
This is the most common and effective method. Instead of stopping all at once, you eliminate one milk removal session every three to five days. This gives your body a chance to recognize the decreased demand and adjust its supply accordingly before you make another change.
- How to Choose: Start by dropping the feeding that your baby seems least interested in, or the one that is most inconvenient for you. Many parents find that the mid-day feeding is a good one to drop first.
- What to Do Instead: During that dropped feeding time, you may need to offer your baby a bottle of formula or expressed milk (if you have it), or solids if they are old enough. It’s also a great time for a cuddle or a distracting activity to redirect their attention.
- Listen to Your Body: Pay attention to how your breasts feel. If after a couple of days you feel overly full or uncomfortable at that time, you might need to hand express just a tiny bit for relief. After 3-5 days, once your body has adjusted and you no longer feel uncomfortably full at that time, you can choose another feeding to drop.
Step 2: Shorten the Duration of Sessions
An alternative (or complementary) approach is to shorten the length of each nursing or pumping session. If you normally nurse for 15 minutes on each side, try cutting back to 12 minutes. A few days later, go down to 10, then 8, and so on. If you’re pumping, reduce your pumping time by a few minutes. This also sends that gentle ‘we need less’ signal to your body without a sudden stop.
Step 3: Hand Express for Relief, Not Removal
This is a critical point! You will feel full and uncomfortable at times. The temptation is to pump or nurse to empty your breasts and feel better. Don’t do it! Emptying the breast is a loud and clear signal to make more milk, which is the opposite of what you want.
Instead, when you feel painful pressure, go to the sink or in the shower and hand express just enough milk to relieve the discomfort. We’re talking about maybe an ounce—just enough to take the edge off. This relieves the pressure that can lead to clogged ducts without stimulating more production.
Managing Comfort and Preventing Engorgement

Managing Comfort and Preventing Engorgement
Even with a gradual approach, you can expect some level of discomfort. Being prepared with a toolkit of comfort measures can make all the difference and help prevent that discomfort from escalating into a bigger problem like a clogged duct.
Your Weaning Comfort Toolkit:
- Supportive, Non-Underwire Bra: A good bra is a must. You want something that provides firm support but doesn’t dig in or constrict breast tissue, as that can contribute to clogged ducts. A comfortable sports bra or a sleep bra worn 24/7 can provide gentle compression and support.
- Cold Compresses: Cold is your friend! It helps reduce inflammation and can numb some of the pain. You can use gel packs from the freezer (wrapped in a thin towel), a bag of frozen peas, or even chilled cabbage leaves.
- Chilled Cabbage Leaves: This is an age-old remedy that many parents swear by. The coolness is soothing, and some believe that an enzyme in the cabbage helps reduce swelling and supply. Wash and chill green cabbage leaves, cut a hole for your nipple if you like, and tuck them into your bra. Replace them when they wilt, usually every couple of hours.
- Over-the-Counter Pain Relief: An anti-inflammatory medication like ibuprofen (Advil, Motrin) can be very effective at reducing both pain and swelling. Acetaminophen (Tylenol) can also help with pain. As always, it’s a good idea to check with your healthcare provider before taking any medication.
- Herbal Teas: Some herbs are thought to help reduce milk supply. Sage tea is the most well-known. You can try drinking a few cups a day. Peppermint and parsley may also have a mild anti-lactation effect. Just be sure to discuss any herbal remedies with your doctor or a lactation consultant.
Remember to stay hydrated by drinking plenty of water, but you don’t need to restrict your fluid intake—that’s an old myth and won’t help you dry up your milk faster.
Recognizing the Red Flags: Clogged Ducts vs. Mastitis
Recognizing the Red Flags: Clogged Ducts vs. Mastitis
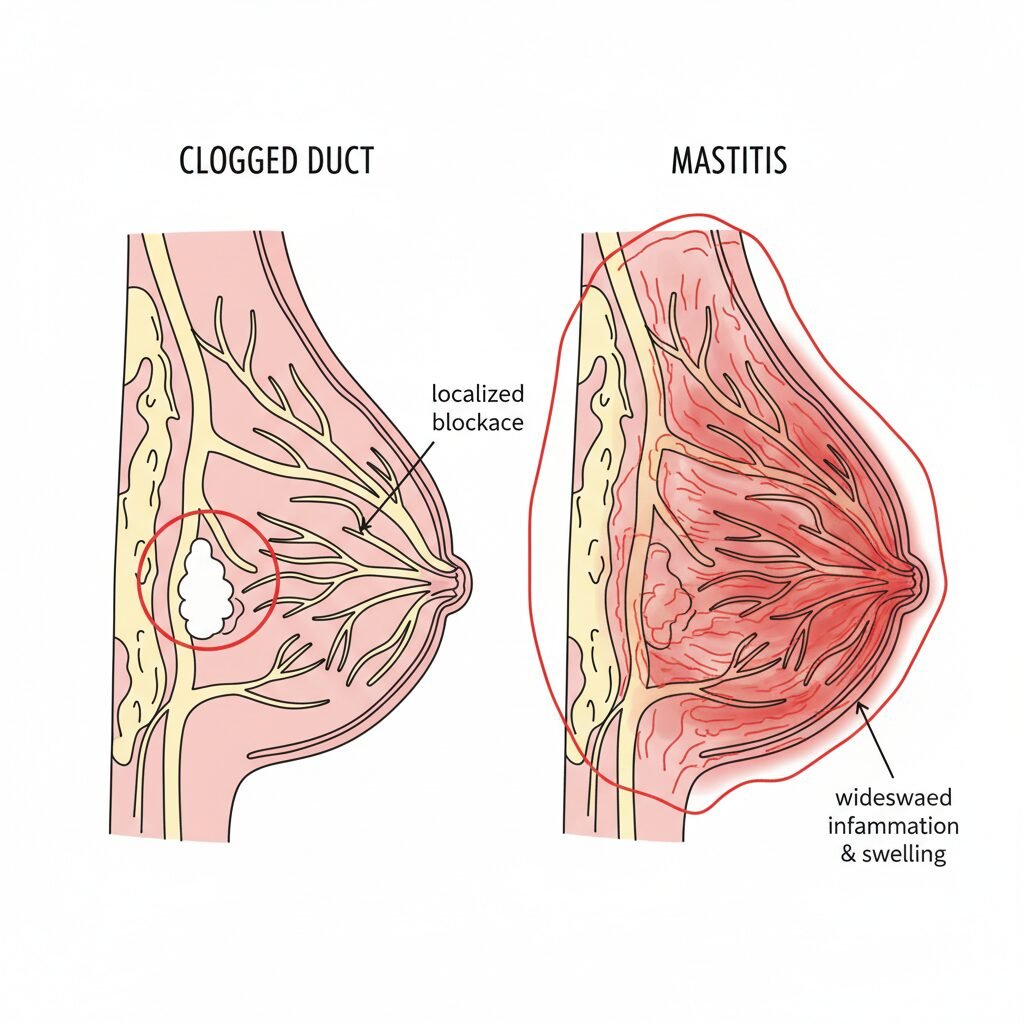
Being vigilant and knowing what to look for is the best way to prevent a minor issue from becoming a major one. A clogged (or plugged) duct is a blockage of milk flow in a specific area, while mastitis is an inflammation of the breast tissue that is often, but not always, caused by an infection.
Here’s how to tell the difference:
| Symptom | Clogged Duct | Mastitis |
|---|---|---|
| Pain/Tenderness | Localized to one specific spot. Feels like a tender, hard lump or wedge. | More widespread pain, swelling, and tenderness affecting a larger area of the breast. |
| Lump/Swelling | A small, firm, and tender lump, often pea-sized or slightly larger. | A larger, hard, swollen, and wedge-shaped area of the breast. |
| Redness & Heat | May have a small, slightly pinkish area over the lump. The area may feel warm. | Often a distinct, red, hot, and swollen patch on the skin. |
| Fever & Body Aches | No fever or systemic symptoms. You feel generally well. | This is the key difference. You will likely have a fever (over 100.4°F or 38°C) and flu-like symptoms: chills, body aches, fatigue, and headache. |
What to Do If You Suspect a Problem
If you find a clogged duct, you need to act quickly to clear it before it can turn into mastitis. The goal is to get the milk flowing through that blockage.
- Apply Warmth: Before nursing or expressing, apply a warm compress or take a hot shower, letting the water run over the affected breast.
- Massage: Gently massage the area, starting from behind the lump and stroking towards the nipple.
- Empty the Breast (Just This Once!): This is the one time you do want to empty the breast. If you’re still nursing, have your baby feed on that side first, positioning their chin to point towards the clog. If you’re not nursing, use a pump or hand expression to drain the breast as best you can.
SAFETY WARNING: If you suspect you have mastitis—especially if you have a fever and feel sick—do not wait. Call your doctor, midwife, or OB-GYN immediately. Mastitis often requires a course of antibiotics, and delaying treatment can lead to a more serious complication like a breast abscess.
Foods, Herbs, and Medications That Can Influence Supply

Foods, Herbs, and Medications That Can Influence Supply
While the primary way to dry up your milk is by reducing demand, certain substances can help speed up the process. However, it’s absolutely essential to approach this with caution and always, always consult your healthcare provider before taking any new medication or supplement.
Things That May Help Decrease Supply:
- Herbs: As mentioned earlier, sage is the most well-known herb for reducing milk supply. You can buy it as a tea or in tincture form. Peppermint, spearmint, parsley, and thyme are also thought to have some anti-lactogenic properties when consumed in larger-than-culinary amounts.
- Pseudoephedrine (Sudafed): This is the active ingredient in some behind-the-counter cold medications. It is known to cause a significant drop in milk supply for many women. You must talk to your doctor or pharmacist before using it, as it’s not suitable for everyone, especially if you have high blood pressure or other medical conditions.
- Hormonal Birth Control: Certain types of hormonal birth control, particularly those containing estrogen, can decrease milk supply. If you are considering starting or changing your birth control method, this is a great topic to discuss with your OB-GYN as part of your weaning plan.
Things to Avoid That Stimulate Supply:
Just as important as what you do is what you don’t do. Avoid anything that sends your body a ‘make more milk’ signal. This includes:
- Excessive Breast Stimulation: This means no long, hot showers with water beating down on your chest, and avoiding any unnecessary nipple stimulation (loose clothing can help).
- ‘Lactation’ Foods and Teas: Steer clear of things known to boost supply, like oatmeal, fenugreek, fennel, and brewer’s yeast. Stop taking any lactation supplements you may have been using.
- Pumping to Empty: It bears repeating! Unless you are trying to clear a clog, do not pump or express until your breasts are empty. Only remove enough to relieve the painful pressure.
Conclusion
My friend, you’ve got this. The journey of weaning is a transition, and like all transitions, it requires patience and a whole lot of grace for yourself. Your body has done an incredible thing, and now it’s time for it to learn a new normal. Listen to its cues, take it one day at a time, and don’t hesitate to lean on your support system. Remember that ending your breastfeeding journey doesn’t diminish the bond you have with your baby one bit. There are endless cuddles, giggles, and moments of connection ahead.
Most importantly, please remember that you are not alone in this. If you are struggling with severe pain, if you’re worried you have mastitis, or if you’re feeling overwhelmed by the process, please reach out to your doctor, a midwife, or a certified lactation consultant. We are here to help you through it safely and compassionately. Be proud of every step of your parenting journey—this one included.







